TRIAGE – Legal Nurse Pearls
by
Jennifer S. Wilson, RN, BS, CEN, CPEN
(Sources for this article are included in the Sidebar.)
Introduction
Triage is derived from the French word trier, which means to sort. It was originally used to describe the sorting of agricultural products. It is now used primarily in health care. Triage is the rapid evaluation process of patient acuity for the purpose of establishing the order and/or location in which the patient should be seen. The earliest documented systems designed to distribute health care among the wounded and sick date back to the military in the 18th century. Napoleon’s chief surgeon recognized the need to categorize wounded soldiers promptly during battle. Injured soldiers were sorted by the severity of their injuries, ranging from those who were severely injured and not salvageable to those who needed immediate care to those who could safely wait. The goal was to return the soldiers to the battlefield as quickly as possible. It was deemed the original 3-level triage system of immediate, urgent, and non-urgent (1). It has since evolved, improving steadily and becoming more refined with each war and through the ongoing years and changes in healthcare (2).
This article will focus specifically on the emergency department (ED) triage algorithm, the Emergency Severity Index (ESI), which is a scientifically validated scoring or rating system. The Emergency Nurses Association (ENA) and the American College of Emergency Physicians (ACEP) promote the use of a standardized screening tool to improve patient care. The ESI is quick and includes standardized screening questions to prevent delays in patient care.
History of Triage Algorithms
The original ESI concept was established in 1998, by two emergency medicine physicians, Richard Wuerz and David Eitel. They formed a group of emergency department nurses, medical practitioners, managers, educators, and researchers, and instituted the ESI algorithm in 1999 (3). It has since been modified and produced in a number of handbooks. In 2012, the Agency for Healthcare Research and Quality (AHRQ) created a Version 4 Handbook, for use of ESI as a triage tool for emergency department care (4). And in 2020, the ENA published the Emergency Severity Index (ESI) Handbook Fifth Edition, Version 5 (5). The ENA handbook serves as a guide, and is best used in conjunction with a comprehensive educational program, along with instruction on institution-specific triage policies and protocols. Triage is most often performed by registered nurses, but can also be performed by other licensed healthcare professionals who have had training. The primary goal of the ESI algorithm is to quickly move the right patient to the right resources, at the right place and time, and is used to coordinate the care and staging of patients in ED waiting rooms via a tracking board or communication device.
There are many other triage algorithms, including the Australasian Triage Scale (ATS) (6), the Manchester Triage System (MTS) (7), and the Canadian Triage and Acuity Scale (CTAS) (8). A noted difference in these algorithms is the monitoring of time intervals for provider evaluation. The ESI system does not define expected time intervals for physician evaluation; however, the ATS scale used in Australia and New Zealand defines the maximum waiting time for medical assessment and treatment. The systems assign ATS1 to patients needing immediate care, and ATS5 to patients who are stable and can wait 120 minutes. The MTS is used in England and Scotland and establishes 5 time intervals: Immediate, Very Urgent (2-10 minutes), Urgent (60 minutes), Standard (120 minutes), and Nonurgent (240 minutes). And lastly, the CTAS scale used in Canada, categorizes the urgency of care into 5 levels of acuity: Resuscitation, Emergent (15 minutes), Urgent (30 minutes), Less Urgent (60 minutes), and Nonurgent (120 minutes).
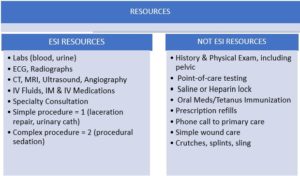
Emergency Severity Index (ESI)
ESI is the most frequently used triage scale in the United States and when used appropriately, improves patient care and outcomes (9). The first question the triage nurse should ask is “does this patient need immediate life-saving interventions?” The assessment begins with an “across-the-room” assessment utilizing the AVPU acronym (alert, verbal, responsive to painful stimuli, or unresponsive):
- Is the patient alert, or is the patient unresponsive? If the patient is unresponsive or only responds to painful stimuli, evaluation is needed immediately and is deemed a level 1, needing immediate life-saving treatment.
- What is the patient’s color? Pale or grey, or nice and pink?
- How is the patient’s breathing efforts? Assessments include airway patency, pulse, cardiac rhythm and rate.
- Is the patient in a high-risk situation, confused, lethargic, disoriented, in severe pain, or one who could easily deteriorate or lose a limb or an organ.
- And lastly, should the patient be evaluated immediately or can the patient wait.
This quick decision making process requires experience and expertise, and experience does not always equal expertise. Some nurses under-triage and some over-triage. Under-triage increases patients’ risks for morbidity and mortality, whereas over-triage limits the resources available to sicker patients. One study involving over 100,000 ED patients, revealed that 22.2% (32,782) were over-triaged and 20.3% (29,996) were under-triaged (10). After assessing the need for immediate life-saving interventions, vital signs are obtained, and if these approach dangerous levels, a higher triage level is considered or assigned, following the established ESI flowsheets. Training, expertise, critical thinking, and excellent assessment skills are necessary components of accurate triage.
An important factor for triage nurses to be aware of, is that triage levels can be eclectic and change with the patient, but ONLY if the patient’s condition changes before they are taken from the waiting room. In this situation, the nurse should carefully document the reason(s) for changing the triage level and the resultant action taken (5). Accurate documentation not only improves patient care, but correct ESI levels inform hospital administration of patient acuity, staff and resource requirements, and bed requirements.
ESI ALGORITHMS
The ENA Emergency Severity Index Handbook Fifth Edition, contains a detailed algorithm for ESI Triage, which includes the following immediate assessments:

LEGAL NURSE CONSULTANT PEARLS FOR REVIEW
When reviewing cases that involve care in an emergency department, legal nurses need to look at the many complexities of triage and the hospital system. Triage is not black and white. It is not an easy process. At any given time, multiple patients may arrive in the waiting room at the same time. Triage nurses needs to look beyond what the patient wrote or said as to the reason they want to be seen. They must ask critical, important questions as to the real reason the patient is there, and determine quickly who gets evaluated first. When reviewing ED cases, legal nurses may look for the following:
- Did the triage nurse quickly determine what is normal and abnormal for the patient – are the symptoms new or have they been present for months?
- Did the triage nurse utilize resources appropriately when indicated, such as call supervisors for additional assistance when needed?
- Did the ED have policies and procedures in place for performing regular, timed reassessments, and did the triage nurse follow the policies and procedures?
- Did the ED have policies in place for direct bedding and ways of communicating to all staff, quickly and effectively when there was an influx of patients?
- What were the hospital’s training guidelines for triage personnel?
- What was the experience level of the triage nurse?
- What is the scheduling process for the ED, are the staff working 12-hour shifts? (Not recommended by the ENA for triage nurses.)
- What ancillary assistance is available in the waiting room? Is there a technician, paramedic or another nurse?
- Who is responsible for transferring patients from the waiting room to the exam room?
- Was there support from nursing supervisors when there was a large influx of patients in the waiting room? Did they help with finding beds for the patients?
- Were labs, imaging, ECG, etc. performed in a timely manner, and did the timing follow hospital protocols? Were the test results reviewed in a timely manner?
- Who does the patient see when they first arrive in the ED? If it is registration, does a triage nurse have full view of the area, in order to perform the across-the-room assessment?
Conclusion
Some EDs have a provider in the triage room with the nurse performing a quick assessment and entering orders. If time allows, some providers may even evaluate and discharge patients directly from the waiting room. Every ED is different. When reviewing cases involving ED admission, legal nurses must determine what policies and procedures were in place at the time of a claimed event, if the policies were followed, and if established triage protocols and algorithms were in place. These are just some of the many questions that need to be asked when reviewing cases involving triage, triage nurses, or emergency department flow.
(Sources for this article are included in the Side Bar.)
Author: Jennifer S. Wilson, RN, BS, CEN, CPEN
Greater Orlando AALNC Chapter, Director at Large
President: J W Legal Nurse Associates
Email: jennifer@legalnurseassoc.com; www.legalnurseassoc.com
Contact: 603-289-7438
_________________________________________________________________________________
CHAPTER MEMBER HIGHLIGHT
JENELLE LEA, MBA, BSN, RN, CEN, GFN-C, SANE-A

Jenelle Lea is a nurse, entrepreneur and avid traveler. She is an actively practicing nurse in the ICU, ER, and Forensic Examiner roles. She has over 31 years of experience as a registered nurse and holds multiple specialty certifications, including Emergency Nursing, Legal Nursing, and Forensics. Her clinical nursing experience includes Intensive Care, Forensics, Emergency Department, and Critical Care Transport. For many years Jenelle managed a large ambulance company and is familiar with Emergency Medical Systems.
Jenelle is the principal founder of SEAL Consulting, a legal nurse consulting practice. She formed SEAL Consulting in 2020 after completing an 18-month ABA approved Legal Nurse Consulting course through the University of California, Riverside. Professionally, Jenelle is an active participant in the American Association of Legal Nurse Consultants, the Emergency Nurses Association, The Academy of Forensic Nursing, and the International Association of Forensic Nurses, holding multiple board member positions through the years.
As a legal nurse consultant, Jenelle enjoys collaborating with both plaintiff and defense attorneys on interesting medical-legal cases within civil and criminal law. Jenelle has been a member of the Greater Orlando Chapter of AALNC since 2022, and is currently serving as a Director at Large. When she is not working, Jenelle is usually planning her next trip!
You can reach her by email at Jenelle@SEALconsulting.com, by phone at 760-522-6222, or through her website SEALconsulting.com
_______________________________________________________________________________
ABOUT THE GREATER ORLANDO CHAPTER OF AALNC
The American Association of Legal Nurse Consultants (AALNC) was founded in 1989, as a not for profit membership organization dedicated to the professional enhancement and growth of registered nurses practicing in the specialty of legal nurse consulting. Chapter development quickly followed. The Orlando community was rich with nurses already practicing in the field of legal nursing. This group of committed professionals quickly became members of the new national organization and recognized the need for a local chapter. The Greater Orlando Chapter of AALNC, founded in 1990, was the second chapter formed under the new national organization. The Chapter was begun in support of AALNC’s mission, by providing networking opportunities, mentoring and support to nurses through professional development and education – a mission that continues today.
______________________________________________________________
MEET THE 2025 GREATER ORLANDO CHAPTER OFFICERS & DIRECTORS

President: Robin Axtell, BSN, RN, LNCC
President Elect: Michelle Gaines, MNA, RN, CRNA
Immediate Past President: Tory Palivoda, BS, RN, LNCC
Secretary: Patty Mitchell, BSN, RN, CLNC
Treasurer: Jillian Talento, BSN, RN, CEN, LNCC
DAL: Pamela Borello, BSN, RN, CNOR, CNAMB, CSSM(e)
DAL: Jill Campbell, BSN, RN, CPTC
DAL: Christine Dorman, DNP, APRN, ACNP-BC, CCRN
DAL: Jenelle Lea, MBA, BSN, RN, CEN, GFN-C
DAL: Lori Mollman, MBA, BSN, RN
CONNECT WITH US
Connect with us on LinkedIn
Check us out at: https://orlandoaalnc.org
Contact us at: info@orlandoaalnc.org
Resources for Critical Confusion Cascade PADIS:
1. Dippenaar, E. Triage systems around the world: a historical evolution, International Paramedic Practice, Vol 9, Number 3, 24 October 2019. https://www.magonlinelibrary.com/doi/abs/10.12968/ippr.2019.9.3.61
2. Iserson, K. V., & Moskop, J. C. (2007). Triage in medicine, part I: Concept, history, and types. Annals of emergency medicine, 49(3), 275–281. https://doi.org/10.1016/j.annemergmed.2006.05.019
3. Wuerz, R.C. Milne, L.W., Eitel D.R., Travers D., & Gilboy, Nicki (1998). Reliability and Validity of a New Five-level Triage Instrument. Academic Emergency Medicine, 2000, 7:236-242. https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1553-2712.2000.tb01066.x
4. Gilboy, N., Tanabe, P., Travers, D., & Rosenau, A. (2012) Emergency Severity Index (ESI), A Triage Tool for Emergency Department Care, Version 4: Implementation Handbook 2012. Quality Agency for Healthcare Research and Quality. file:///D:/Downloads/GOVPUB-HE20_6500-PURL-gpo23161-1.pdf
5. Emergency Severity Index (ESI) Handbook Fifth Edition, Version 5, Emergency Nurses Association, Copyright 2023. file:///D:/Downloads/Emergency_Severity_Index_Handbook-1.pdf
6. The Emergency Triage Education Kit, Australian Government Department of Health and Aged Care (2024) Endorsed by College of Emergency Nursing Australasia Ltd and Australasian College for Emergency Medicine. https://www.safetyandquality.gov.au/sites/default/files/2024-04/emergency_triage_education_kit_-_second_edition.pdf
7. Understanding the Manchester Triage System. https://sonder.io/resources/blog/manchester-triage-system/
8. The Canadian Triage and Acuity Scale: Education Manual, Version 2.5, 2012. file:///D:/Downloads/module_1_slides_v2.5_2012.pdf
9. Yancey CC, O’Rourke MC. Emergency Department Triage. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2025. PMID: 32491515. https://www.ncbi.nlm.nih.gov/books/NBK557583/
__________________________________
CALENDAR OF EVENTS

Be sure to check out the AALNC calendar of events, which includes MANY events, presented by ALL of the AALNC Chapters and by AALNC! You can fill your calendars for the rest of 2025! And mark your calendars for the Greater Orlando Chapter Update and CE Webinar Dates for the remainder of 2025:
- September 16, 2025 – “IME/DME – The LNC Role”
- October 21, 2025 – Presentation on Abdominal and Thoracic Aortic Aneurysms
- November 18, 2025 – The Nurse Expert Witness – Winning the Case
Don’t forget our On-Demand Webinars. We have 20 On-Demand Webinars which are free for Chapter members and only $20 for non-Chapter members.
And check out the education programs from our fellow AALNC Chapters:
- Bay Area Chapter of Northern California at: https://www.bacnc.org/
- New Jersey Chapter at: https://aalncnjchapter.clubexpress.com/
- Pittsburgh Chapter at: https://aalncpittsburgh.org/
- Tampa Bay Chapter at: https://www.aalnctampa.com/
- Pacific Northwest Chapter at: https://www.pnw-aalnc.com/
CONTINUING EDUCATION INFO
The Greater Orlando Chapter of AALNC is an approved provider of Nursing CE through the Florida Board of Nursing and CE Broker, and approved by the following States: Arkansas, District of Columbia, Florida, Georgia, Kansas, Kentucky, Mississippi, New Mexico, South Carolina and West Virginia. We report CE directly to CE Broker in these states. For attendees from other States, we provide required documents for self-reporting CE to State Boards of Nursing.
____________________________________
LNC LAUNCHPAD – Q&A with Greater Orlando Chapter LNCs
In 2021 we started a new program for members, which we call “LNC Launchpad – Q&A with Greater Orlando Chapter LNCs.” This is a 1.5 hour session to provide guidance, answer questions, and suggestions. We limit the event to 10 participants, so we can mentor each attendee – whether new to the LNC practice or experienced and ready for a change – we are there for you! We have the 2025 dates selected so plan ahead, the slots fill up fast! (Registration for the May 2025 session will open mid-April, 2025.)
- September 9, 2025
- November 4, 2025

LNC PROFESSIONAL DEVELOPMENT
AALNC and the Chapters are THE GO TO sources for networking and professional development in the field of legal nurse consulting. Want to learn of career opportunities? Want to stay up to date with the LNC industry trends? Want to hone your LNC skills and learn new ones? Then go to AALNC at https://aalnc.org and join now! Then go to https://orlandoaalnc.org and join our Chapter! And you can join ALL of the AALNC Chapters – for unlimited networking and LNC education!
WE ARE NEAR YOU! Maybe not geographically, but through your computer or phone. The Greater Orlando Chapter has members in 33 States. SINCE 2014, The Greater Orlando Chapter’s live Chapter Meetings with CE Programs have been broadcast virtually! So members and guests have been attending from all over the Country since then! Because of COVID, since 2020 all of our CE Programs have been virtual only. And though our Chapter Update Meetings and CE Programs are virtual, we have Chapter Socials and we hope our members from all over the Country find their way to Florida for some warm, sunny weather and a lot of LNC networking! We just had our first 2025 in-person Social on March 29, 2025! It was awesome. Out next opportunity to see our member is person will be in April 2026, at the AALNC Forum in Orlando. More about this exciting event below!
If You Have Questions, Contact Us:
Email us at: info@orlandoaalnc.org
Or visit us at: https://orlandoaalnc.org
___________________________________
AALNC UPCOMING EVENTS YOU DON’T WANT TO MISS:
LNC JUMPSTART 2025

If you have not already registered for LNC Jumpstart, you still have time. The next live session (workshop) is September 12, 2025! Jumpstart provides a wealth of information for new LNCs as well as those expanding their practice! To register, go to https://www.aalnc.org/Events/LNC-Jumpstart.
_________________________________

March 2026 is going to be AWESOME!
AALNC Annual Forum is going to be a live event again in 2026, and it will be in BEAUTIFUL Orlando! AALNC has partnered with AANLCP for what promises to be a Forum for the record books! Go to https://www.aalnc.org/Events/AALNC-Annual-Forum for more exciting information.
___________

